For those navigating the maze of digestive discomfort, the terms diverticulitis and hemorrhoids often spark a mix of confusion and concern. Diverticulitis is the inflammation of diverticula (small pouches) in the colon and or large intense, while hemorrhoids are swollen veins located near the rectum and anus.
Although diverticulitis and hemorrhoids are separate and distinct conditions affecting different parts of the body, new research has shown that they actually may be related in that those who have diverticulitis often suffer from hemorrhoids. Understanding each condition and what each of their symptoms are, is key to knowing their connection as well as managing and preventing them.
Hemorrhoids: Causes and Symptoms
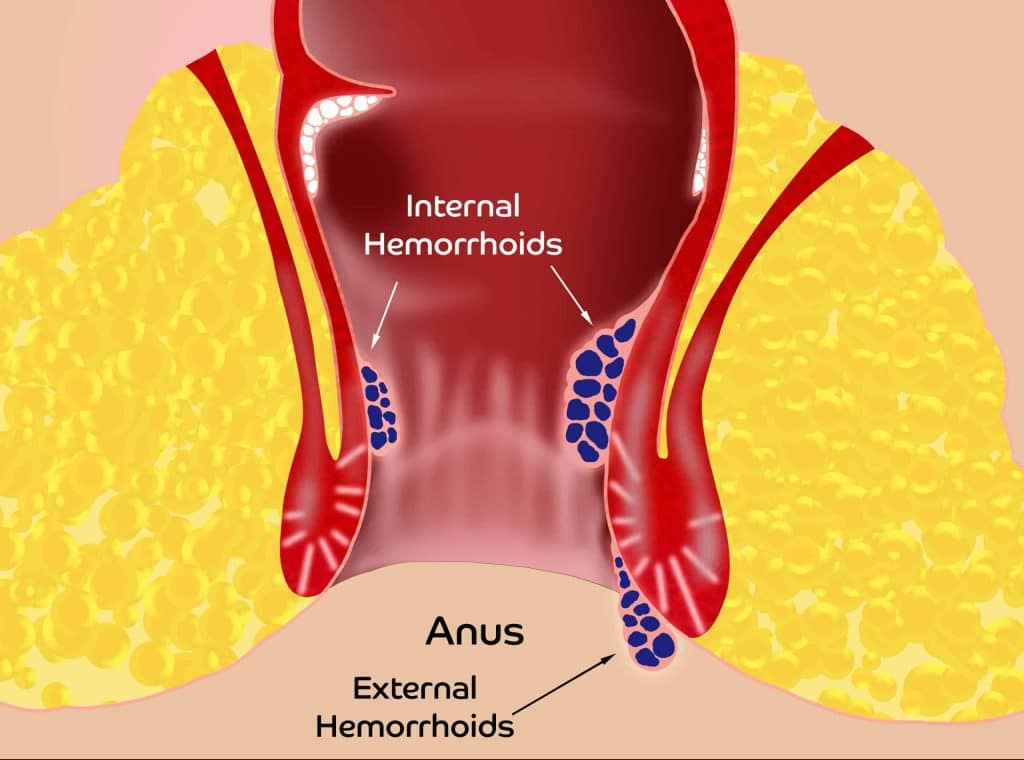
Hemorrhoids are veins which reside inside and outside of the anus. They are organs just like lungs, heart, kidneys and spleen are organs. Hemorrhoids are venous cushions which have a blood supply (artery which pumps blood into the hemorrhoid) and a venous return (veins which return the blood to the body). They are a part of our anatomy just like our eyes, nose, ears, toes, etc.
We are born with at least 6 hemorrhoids, three within the anus (internal hemorrhoids) and three outside the anal opening (external hemorrhoids). Though we have theories as to the function of hemorrhoids, there is no real scientific evidence of their purpose. It is proposed that the function of hemorrhoids is to aid in keeping stool from leaking out of the anus.
When hemorrhoid veins become inflamed and enlarged they can become symptomatic. The blood pumped into the hemorrhoid is thin and normal, but when the blood enters the inflamed hemorrhoid the inflammatory proteins made by the body thicken the blood so it is difficult to leave the hemorrhoid. This is called chronic venous insufficiency (CVI). With CVI there is more blood leading into the hemorrhoid than returning to the body. Think of a water balloon on a faucet but the balloon has tubes allowing water to flow back to the system. If the water coming into the balloon becomes thick like maple syrup, more water will enter the balloon than will leave the balloon so the balloon becomes bigger. As hemorrhoids become larger they start to cause symptoms.
There are several reasons why hemorrhoid symptoms develop, such as:
- Straining during bowel movements due to constipation
- Urgency to have a bowel movement – diarrhea
- Sitting for long periods of time
- Obesity
- Pregnancy
- Aging
- Chronic bowel issues
- A family history of hemorrhoids.
Symptoms of hemorrhoids:
The symptoms of hemorrhoids include internal hemorrhoid symptoms and external hemorrhoid symptoms. Though patients may experience pain, this pain is a throbbing, aching, toothache type pain, which is different from a fissure pain that tends to be sharp.
Internal hemorrhoid symptoms:
- Throbbing, aching pain around the anus
- Itching
- Painless bleeding
- Anorectal pressure
- Prolapse, a protrusion outside of the anus
- Urgency or the feeling of having to have a bowel movement but no stool comes out
- Mucous discharge
- Necrosis; when the hemorrhoids become trapped outside the anus and the hemorrhoid tissue starts to die). This is a surgical emergency.
External hemorrhoid symptoms:
- A clot within the hemorrhoid, called thrombosis, which causes pain, itching and sometimes bleeding with clots, if the hemorrhoid ruptures. A painful swollen lump that looks like a purple grape is a thrombosed hemorrhoid. 95% of the time thrombosed hemorrhoids will resolve on their own and recurrence in the same spot is unlikely therefore only conservative therapy is needed.
- Necrosi, a condition when the external hemorrhoid becomes thrombotic and due to the pressure in the hemorrhoid the tissue starts to die. This is a surgical emergency and needs immediate medical attention.
- Swelling without clotting
While hemorrhoids can be uncomfortable, they can often be managed with lifestyle changes, dietary adjustments, and over-the-counter treatments such as topical creams, ointments, or suppositories. In more severe cases or when conservative measures fail to provide relief, medical procedures like rubber band ligation or sclerotherapy may be recommended by your proctologist.
What Is Diverticulitis and What Causes It
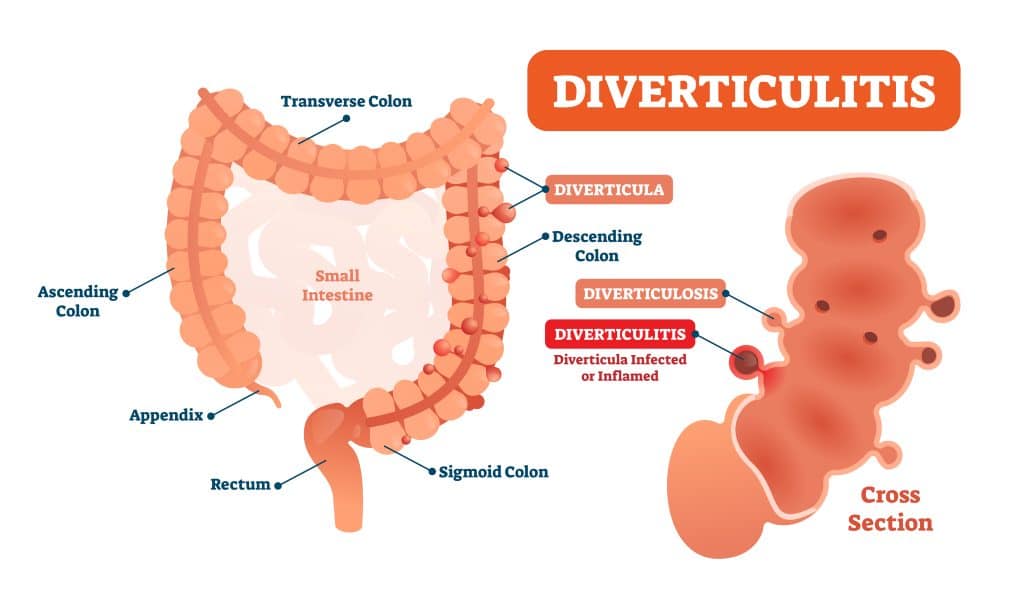
Diverticulitis is a condition characterized by inflammation or infection of small pouches, called diverticula, that form in the lining of the colon or large intestine. These pouches, known as diverticula, can develop over time due to increased luminal pressure within the colon, typically from factors such as constipation or diarrhea, both of which increase luminal pressure. This increased pressure within the colon causes the inner lining, also called “mucosa” to bulge outward through the lining of the colon forming diverticula, this is known as diverticulosis.
The exact cause of diverticulitis is not fully understood, but several factors may contribute to its development:
- Low-fiber diet
- Age
- Genetics
- Lifestyle factors
- Lack of physical activity
Symptoms of diverticulitis
- Abdominal pain, usually on the left side
- Fever
- Nausea and vomiting
- Diarrhea
- Bloating or gas
- Tenderness in the abdomen (usually left lower quadrant), especially when touched
Treatment for diverticulitis typically involves antibiotics to treat the infection, along with dietary modifications such as a clear liquid or low-fiber diet to allow the colon to rest. In some cases, hospitalization and surgery may be necessary, especially for complications or recurrent episodes.
The Potential Relationship Between Diverticulitis and Hemorrhoids
It is possible that patients with diverticulitis may also experience episodes of hemorrhoids, which could suggest a relationship between the two conditions, but more research is still being conducted on the topic.
One potential connection between these two conditions lies in their shared risk factors and symptoms. Both diverticulitis and hemorrhoids can be influenced by factors such as diet, age, and bowel habits. For instance, constipation, a common symptom of diverticulitis, can also contribute to the development of hemorrhoids by straining the rectal veins during bowel movements. Additionally, the increased pressure within the colon during diverticulitis flare-ups may exacerbate existing hemorrhoids or contribute to their formation.
However, despite these potential links, it’s important to note that diverticulitis and hemorrhoids are distinct conditions with different underlying causes and mechanisms. Diverticulitis involves inflammation or infection of the diverticula, while hemorrhoids involve swelling of the rectal veins. While diverticulitis may indirectly influence the development or worsening of hemorrhoids, it is not typically considered a direct cause.
Further research is needed to fully understand the relationship between diverticulitis and hemorrhoids. This includes investigating the potential mechanisms through which diverticulitis may contribute to hemorrhoid development or exacerbation, as well as exploring strategies for managing both conditions simultaneously. In the meantime, healthcare providers should remain vigilant in identifying and addressing the unique needs of patients with either diverticulitis, hemorrhoids, or both.
Managing and Preventing Hemorrhoids and Diverticulitis

Although they may not be directly related, managing hemorrhoid and diverticulitis share similar lifestyle modifications and dietary changes to help promote digest health and reduce symptoms.
Some strategies to manage and prevent both conditions include:
- High-fiber diet like psyllium to bulk the stool. This lowers intraluminal colon pressure and anal pressure both of which decrease the risk of developing diverticula and hemorrhoids. The best psyllium on the market is PERFECT P.O.O.P. RAW, VEGAN psyllium fiber.
- Hydration – drink at least 4-6 eight ounce glasses of water per day or more if exercising. Caffeine and liquor are diuretics which increase urination causing dehydration. Therefore, coffee, tea, caffeinated sodas, and liquor do not count as water. For every cup of coffee or tea drink an extra glass of water. Drinking water with each meal will add 3 glasses of water a day.
- Regular exercise
- Healthy weight
- Avoid straining on the toilet
- Fiber supplements
- Regular check-ups
By incorporating these lifestyle changes and strategies into your daily routine, you can help manage symptoms and reduce the risk of developing hemorrhoids and diverticulitis. However, if you experience persistent or severe symptoms, it’s important to seek medical attention for proper diagnosis and treatment.

