Among the many conditions that can affect your gut, two terms frequently come up that can be confused: diverticulosis and diverticulitis. While they sound similar and are closely related, they describe two distinct processes associated with a common intestinal issue. These two conditions combined are called diverticular disease.
What is Diverticulosis?
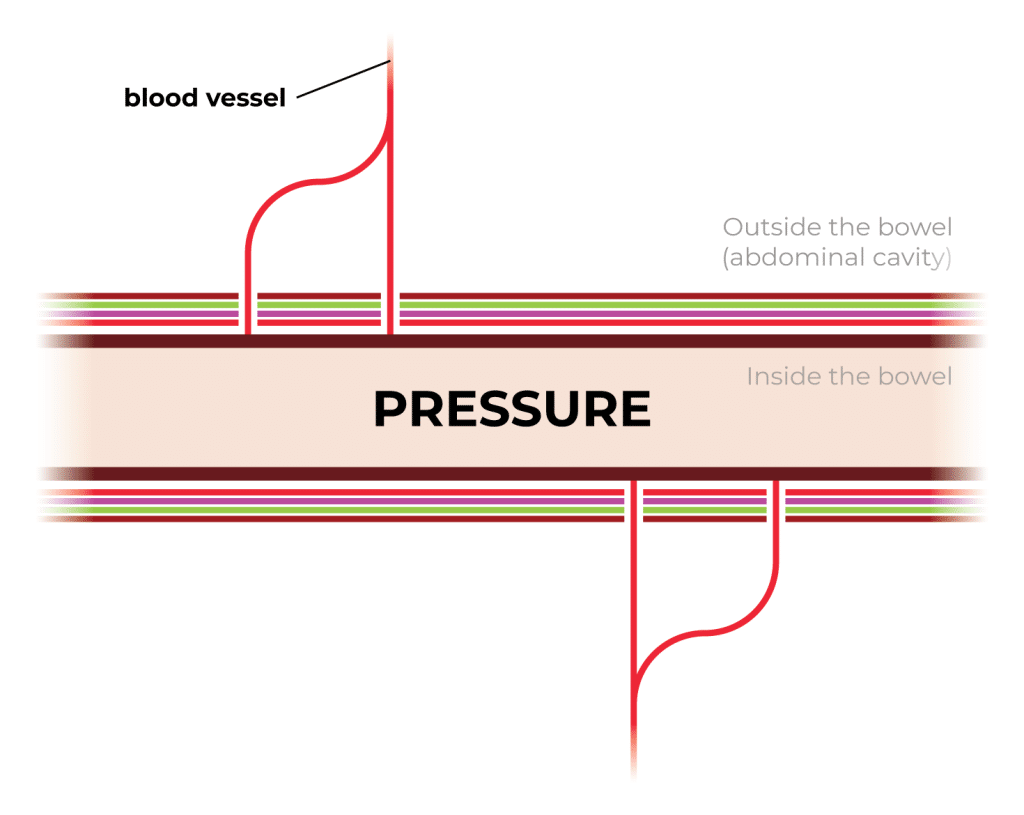
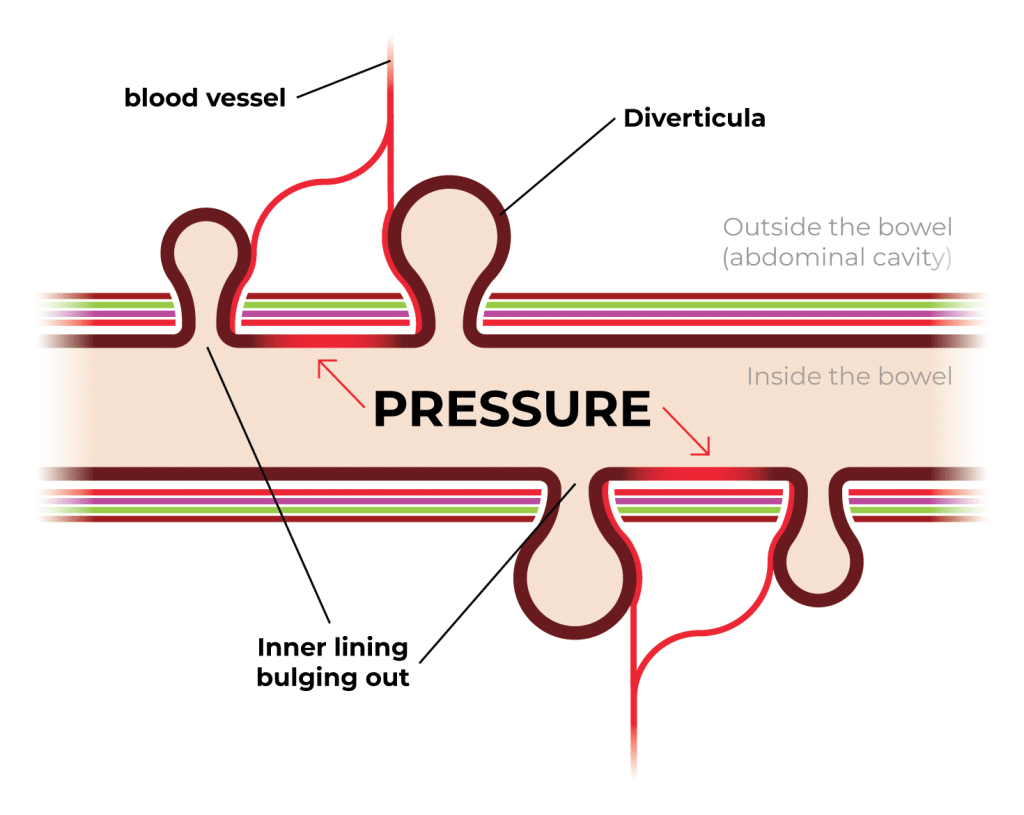
Diverticulosis is when small pockets, called diverticula, form along the walls of your colon due to pressure. They can develop anywhere in the digestive tract, but most often occur in the colon. These pockets are like tiny balloons pushing through a weak spot. The pressure causes the inner lining of the colon, the mucosa, to bulge outward past the outer layer of the colon called the serosa. This pressure is mainly caused by a lack of fiber content, leading to smaller, firm stools, which require the colon to squeeze harder to move the firm stool along.
They are usually harmless on their own, develop at an older age, and many people experience little to no symptoms. It’s estimated that about 50% of people over the age of 60 have diverticulosis. It is often found accidentally during a colonoscopy or imaging test for another condition.
What is Diverticulitis?
Diverticulosis develops into diverticulitis when the diverticulosis pockets become inflamed and progress to an infection. Only about 10-25% of people with diverticulosis will develop diverticulitis.
While diverticulosis can be benign and symptomless, diverticulitis is an active disease state that typically demands medical attention. It ranges from mild inflammation to severe infections, abscesses, or even mass fecal spillage into the abdomen (feculent peritonitis).
What Causes Diverticular Disease?
While research isn’t firm on the causes of colonic diverticulosis formation, most research points towards lifestyle factors, especially modern diets that tend to be low in fiber. Since fiber helps keep stools soft and easy to pass, a diet low in fiber can lead to constipation. Frequent constipation increases pressure in the colon, contributing to the formation of diverticula.
Other factors include sedentary behavior, poor gut health, smoking, and obesity. Like many medical conditions, it is also thought to be simply based on genetics in some cases.
Diverticulosis vs Diverticulitis Symptoms
Knowing the symptoms of diverticulosis and diverticulitis can help you catch issues early and seek the right care. Although they sound alike, the signs of each can look very different depending on whether inflammation or infection is involved.
Symptoms of diverticulosis include:
- Excessive gas and bloating
- Crampy, intermittent left lower quadrant abdominal pain
- Massive GI bleeding
- Constipation and diarrhea
Symptoms of diverticulitis include:
- Fever and chills
- Nausea and vomiting
- Persistent pain or tenderness in the lower left side of the abdomen
- Abdomen distension
It’s also worth noting that some symptoms, like blood in the stool or abdominal pain, can overlap with other conditions like hemorrhoids.

Diverticulosis vs Diverticulitis Diagnosis & Testing
Accurately diagnosing diverticulosis or diverticulitis can be done in the office if the symptoms are mild. If symptoms are more severe, an emergency room visit with a radiology examination and labs are needed. Because symptoms can overlap with other conditions, proper testing is essential to determine the exact cause and guide treatment.
Here’s how doctors typically identify each condition.
- If a patient has mild symptoms and abdominal tenderness on examination, diverticulitis is the likely diagnosis. In cases where a prior colonoscopy has shown diverticulosis, the likelihood of diverticulitis is even higher. If the patient has not undergone a colonoscopy, it is recommended to perform one after the symptoms have resolved, typically about six weeks later, to allow the inflammation to subside.
- For patients with severe pain and fever a CT scan is beneficial for identifying diverticulitis and its severity. A CT scan can diagnose both uncomplicated diverticulitis (inflammation) and complicated diverticulitis, such as an abscess, perforation, or fistula formation.
- Colonoscopy: Typically used when diverticulitis is not active to assess for diverticulosis
- Ultrasound or MRI: Sometimes used in place of CT, especially for younger or pregnant patients
It’s important to note that if you have active diverticulitis, a colonoscopy is usually postponed for about six weeks after the inflammation has subsided to avoid the risk of perforation.
Diverticulosis Treatment & Prevention
Since diverticulosis is a non-threatening condition, the key to treatment is focused on possible prevention and managing symptoms. While nothing is proven to prevent the formation of diverticulosis or reduce symptoms, some tips that might help include:
- Increasing the amount of fiber in your diet by incorporating more green vegetables, whole grains, and other high-fiber whole foods. Aim for at least 25-30 grams of fiber per day. I recommend PERPECT P.O.O.P. raw psyllium fiber as an amazing and easy way for patients to boost their fiber intake. Psyllium is nature’s best fiber, creating a long, solid, soft, and clean bowel movement.
- Moderate use of laxatives to combat constipation symptoms
- Increase water intake
- Regular exercise
- Avoid smoking
- Although no evidence-based studies show that certain foods cause diverticulitis, it is suggested to avoid foods like nuts, seeds, and popcorn. I personally don’t recommend cutting these foods out to my patients with diverticulosis.
Diverticulitis Treatment Options
While diverticulosis isn’t a major concern, diverticulitis requires immediate medical attention due to the presence of a bacterial infection. In some severe cases, complications such as bowel obstruction, fistulas, or peritonitis (a potentially life-threatening abdominal infection) can occur.
Treatment options for diverticulitis include:
- Antibiotics and/or pain medication
- Bowel rest for 2 weeks, which includes a soft to liquid diet and no solid food
- Surgery may be necessary if the infection doesn’t subside, complicated diverticulitis is diagnosed (such as abscess, fistula formation, or bowel perforation), or the patient experiences persistent or recurrent attacks of diverticulitis
- In rare cases, a colostomy bag may be fitted to allow the colon to heal
After recovery, many patients are advised to adopt a high-fiber diet to prevent recurrence and to follow up with a colonoscopy to rule out other conditions like colorectal cancer.
Foods to Avoid with Diverticulitis
Balancing a diet with diverticulitis can be complex. While a fiber-rich diet is essential for preventing the infection of diverticula, once the infection sets in, high-fiber foods are your worst enemy. Foods to avoid with diverticulitis include:
- Beans
- Brown rice
- Red meat
- Fried and/or greasy foods
- Spicy foods
- Raw fruits and vegetables
- Nuts and seeds
Avoiding the wrong foods during a diverticulitis flare-up can make a big difference in how quickly you recover. Once symptoms improve, your doctor may gradually reintroduce fiber and other nutritious foods to help prevent future episodes.
Diverticulosis vs Diverticulitis: Take Charge of Your Gut Health
Understanding the difference between diverticulosis and diverticulitis is vital for recognizing symptoms, seeking the right treatment, and making lifestyle changes that can protect your long-term health. If you’ve been diagnosed with diverticulosis, don’t panic. It doesn’t automatically mean you’ll develop diverticulitis. Diverticulosis on its own is very common and can be easily managed. If it becomes infected or inflamed, emergency medical attention is needed. If you suspect diverticulitis, contact our team at Thousand Oaks Proctology to schedule an appointment today. We’ll help you get to the bottom of your problems with compassionate care.

