Facing your first colonoscopy often comes with a mix of uncertainty and hesitation. Some people question whether or not they really need one. With colorectal cancers on the rise, especially in younger people, getting your digestive health checked out is the best form of prevention.
In this article, we provide a comprehensive guide to colonoscopies to help you feel better informed about your health decisions.
What is a Colonoscopy?
A colonoscopy is a diagnostic exam performed by a medical professional, typically a proctologist or a gastroenterologist, to identify any abnormalities in your large intestine, including the colon, rectum, and anus.
A colonoscope is a long, flexible tube with a light and a tiny camera on the end. The scope is gently inserted into the anus and guided through the rectum and entire colon to look for polyps, inflammation, or other signs of colorectal cancer. During a colonoscopy, polyps and irregular tissue can be removed for further testing.

Why Should You Have a Colonoscopy Screening?
Colonoscopy screenings detect colorectal cancer, precancerous growths, and other gastrointestinal issues. Screenings are critical for cancer diagnostics and prevention because they detect and remove abnormalities in a single procedure. A colonoscopy decreases the mortality rate from colon or rectal cancer by 52%. No other test has these results.
Qualifications for a colonoscopy screening include:
- Adults aged 45 and older who have no symptoms of colorectal cancer and no personal or family history of colorectal cancer or precancerous polyps.
- If it has been 10 years since a normal colonoscopy.
Qualifications for a colonoscopy for moderate to high-risk individuals include:
- A personal history of precancerous polyps
- A personal history of colon or rectal cancer
- A family history of colon cancer or precancerous polyps
- A genetic predisposition for colon and rectal cancer, such as Hereditary Nonpolyposis Colon Cancer Syndrome (HNPCC) or Familial Adenomatous Polyposis syndrome (FAP)
- Symptoms of colon or rectal cancer:
- Bright red bleeding
- Black tarry stool (Melena)
- Purple stool or blood in the stool (Hematochezia)
- Unusual abdominal pain
- Change in stool caliber to a much thinner stool
- Unexplained anemia (blood loss)
- Unexplained weight loss
How to Prepare for a Colonoscopy
Properly preparing for a colonoscopy is key to a successful screening. Your doctor will provide instructions on how to prepare, which involves cleansing your colon. If your colon is not cleaned out, the camera might not capture the necessary images needed for a complete assessment.
There are many colonoscopy bowel preparation instructions online. My recommendation is to follow your doctor’s instructions, not any others you may see online. Inadequate preparation can make the test less effective, and you may need to repeat it within six months.
Preparation usually involves:
- Bowel prep: Drinking a prescribed laxative solution the day before and early in the morning of the procedure, usually six and a half hours before the procedure. I can always tell when my patients have followed my preparation instructions closely. They come in tired, hungry, irritable, and sick of drinking the bowel preparation.
- Diet adjustments: Follow a clear liquid diet (your doctor’s instructions will list clear liquids) for 24 hours before, and avoid certain foods for a few days beforehand. I personally don’t allow Jell-O during prep, as it contains collagen derived from bone, which isn’t fully digestible and therefore doesn’t qualify as a true clear liquid.
- Medication adjustments: Some medications, especially blood thinners or diabetes medications, may need to be temporarily paused (always follow medical advice).
- GLP-1 medicines need to be stopped for a week before a colonoscopy as they slow down gastric emptying, increasing the risk of aspiration during anesthesia.
During Your Colonoscopy
For all of my patients, after checking into the outpatient center, you’ll prepare for the procedure by changing into a hospital gown. A nurse will start an IV, and you’ll meet with the anesthesiologist. I’ll also stop by to see if you have any last-minute questions before we get started.
You’ll then be taken to the GI suite, where the anesthesiologist will administer a twilight anesthesia. This type of sedation allows patients to sleep comfortably through the procedure. They feel nothing, remember nothing, and breathe on their own without the need for a breathing tube (general anesthesia). Patients wake up feeling alert, rested, and without nausea or grogginess.
Some gastroenterologists or proctologists do not use an anesthesiologist and instead administer their own sedation, typically a combination of Versed and Fentanyl. These medications take longer to take effect and can leave patients feeling groggy or nauseated afterward. I personally always work with an anesthesiologist so I can stay fully focused on performing the colonoscopy and ensuring a thorough examination.

Once the procedure begins, the colonoscope is gently inserted into the anus, and air, water or carbon dioxide is used to expand the colon for better visibility. Your doctor will guide the camera through the rectum and then advance it to the sigmoid colon, the descending colon, the splenic flexure, the transverse colon, the hepatic flexure, the ascending colon, and into the cecum (the beginning of the colon).
I personally advance slightly into a small portion of the terminal ileum, or small bowel, to inspect for any abnormalities. If polyps or abnormal tissue are found, they will be removed (polyps) or biopsied (inflammation or a mass) during the examination. Overall, the procedure should take between 20 to 30 minutes.
After Your Colonoscopy
When the procedure is complete, you will rest in a recovery area until your sedation wears off. Patients who receive anesthesia from an anesthesiologist typically feel fully awake within about 15 minutes, while those whose endoscopist administers the sedation may take 30 to 60 minutes to feel back to normal.
You’ll need someone to drive you home and should avoid driving the rest of the day, even if you feel fine later on. Most patients can resume their normal activities the next day. Mild bloating or cramping is common afterward due to the air introduced during the procedure. When carbon dioxide is used instead of air, these symptoms are uncommon since the gas is absorbed by your body and released naturally as you exhale.
What Your Colonoscopy Results Mean
In most cases, you will receive your results right away. When you are in recovery, your doctor will explain how it went and what they found. Below are the different results from a colonoscopy, along with their interpretation. Next steps, if any, will be discussed with your healthcare provider.
- Normal: No abnormalities found.
- Polyps found: The type, size, and quantity determine when you should have your next colonoscopy (often 3–5 years).
- Other findings: Inflammation, diverticulosis, or cancer may be detected, leading to follow-up treatment.

Colonoscopy Risks
Colonoscopies are very safe and the risks are minimal, but like any medical procedure, it has potential risks:
- Bleeding (especially after polyp removal)
- Perforation (tear in the colon wall)
- Reaction to anesthesia
- Infection (extremely rare)
- Missing polyps or cancer
Alternatives to Colonoscopies
While colonoscopies are the most effective method for identifying abnormalities in the large intestine, there are alternatives for those who prefer not to undergo the procedure.
Cologuard
Cologuard is a non-invasive test that detects abnormal DNA and blood markers associated with colon cancer using a simple stool sample, which can be collected in the comfort of your own home.
- Pros: No prep, non-invasive, can be done at home.
- Cons: Much less accurate for detecting precancerous polyps, which is the goal of a screening test. If you get an abnormal result, it’s not known if a polyp or a cancer was the cause, and you will need to have a colonoscopy to find out.
Virtual Colonoscopy (CT Colonography)
A virtual colonoscopy, also known as CT colonography, uses CT scans to create images of the colon to identify polyps or abnormalities.
- Pros: Less invasive, no sedation required.
- Cons: This option still requires bowel prep and exposes the patient to radiation from the CT scan. If abnormalities are found, a traditional colonoscopy is needed for removal and biopsies, which requires another bowel preparation.
Fecal Occult Blood Test (FOBT)
This is when stool is collected, placed on a special paper and evaluated for blood.
- Pros: Less invasive, no sedation, no bowel preparation.
- Cons: Less accurate than colonoscopy, high false positive (the test is abnormal and the colonoscopy is normal), required yearly along with a flexible sigmoidoscopy every 5 years. Certain foods and non steroidal anti-inflammatory agents need to be stopped as they can cause an abnormal result.
Fecal Immunohistochemical Test
Fecal Immunohistochemical Test is a test that checks a small stool sample for hemoglobin.
- Pros: Less invasive, no sedation, no bowel preparation. No need to stop NSAIDS or dietary restriction. More accurate than FOBT for finding cancer.
- Cons: Less accurate than colonoscopy for finding polyps. If abnormal a colonoscopy is needed.

Pros to a Colonoscopy vs Alternatives
A colonoscopy offers several key advantages over the alternatives:
- Most accurate for identifying polyps, which can be removed immediately.
- Depending on your risk factors, like age and family medical history, you will only need a colonoscopy every 5-10 years.
- Most accurate and effective test available.
- Reduces mortality from colon and rectal cancer by 52%.
Alternative screening options are appealing because they are:
- Non-invasive and have no immediate risks (no sedation, no scope, etc).
- Convenient and less time-consuming.
Colonoscopy FAQs
How long does a colonoscopy take?
Typically 20-30 minutes, but expect to spend 1.5-2 hours at the facility, including procedure prep and recovery.
What can I eat before a colonoscopy?
Your doctor should discuss with you how to prepare for your colonoscopy, including your prescribed laxative solution and the clear liquids approved for preparation. A few days before, avoid certain foods to ensure a successful procedure. Be sure also to avoid red or purple liquids, since they can look like blood during the exam.
How much does a colonoscopy cost?
Costs for a colonoscopy vary widely, but the average is $2,750 in the U.S. They are often covered by insurance as a preventive service if you meet the requirements. If you do not have insurance, there are nonprofit organizations that might help with the cost of the procedure as well.
Does a colonoscopy hurt?
Most people don’t feel pain due to sedation. Some patients experience mild cramping or bloating afterward.
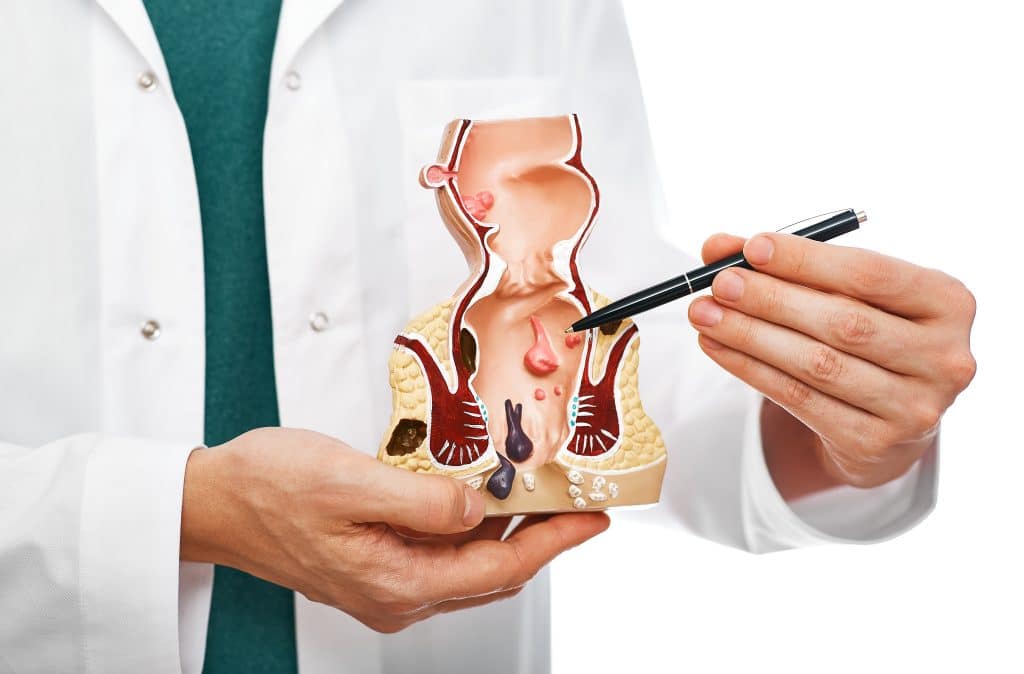
What does a colonoscopy show?
A colonoscopy can detect polyps, cancers, ulcers, diverticulosis, inflammation, and signs of colitis.
Is a colonoscopy a surgery?
A colonoscopy is considered an invasive procedure because the colonoscope enters the body cavity. In reality, if a biopsy or polyp removal (polypectomy) is performed, it technically qualifies as surgery, since surgery is defined as cutting tissue with an instrument.
That being said, when we consider surgery, we usually think of cutting tissue in areas rich in nerve endings, which usually requires a painful recovery. The recovery after a colonoscopy with a biopsy or polypectomy is the same as after a routine colonoscopy. There is typically no pain afterward.
What age should you get a colonoscopy?
Colonoscopy screenings are generally recommended to begin at age 45 for adults at average risk. If you have concerning symptoms or family history of colorectal issues, you may need to start earlier. Talk to your doctor to determine the right timeline for you.
How often should you get a colonoscopy?
If your screening colonoscopy results are normal, you should schedule one every 10 years. If polyps were found or you’re considered high risk, more frequent screenings may be necessary. Your proctologist will recommend the best course of action for your specific case.
What kind of doctor performs a colonoscopy?
A proctologist or a gastroenterologist usually performs colonoscopies. A proctologist, or colorectal surgeon, is a doctor who specializes in conditions of the anus, rectum, and colon. A gastroenterologist is a specialist in the digestive system.

Why a Colonoscopy is a Smart Step for Your Health
A colonoscopy is one of the most effective tools for preventing colorectal cancer and detecting other gastrointestinal conditions. While alternatives can be helpful, colonoscopies will leave you with no unanswered questions. Rectal bleeding is the most common symptom requiring a colonoscopy for patients under 45 years of age. If you have any bleeding, see your doctor to schedule a colonoscopy. If you’re approaching 45 or have other risk factors, taking this step now can save your life later.
Don’t wait for symptoms to appear. Most early-stage colorectal cancers have none. Proactive screening gives you peace of mind, clarity, and control over your future. If you’re ready to prioritize your health, contact us today to schedule your first colonoscopy. We’re committed to providing a warm, caring, and passionate environment for every patient.

