How to Heal a Fistula Without Surgery
Non-Medicated Seton Placements (Cutting and Non-Cutting Setons)
Fistulas, caused by severe inflammation, are common in Crohn’s disease patients. Seton placements treat Crohn’s related anal fistulas, although some patients prefer a non-cutting seton. This is when a patient spins a small piece of surgical thread through the fistula. The thread is placed along the tract and pushes the wound to the surface.
The goal is to stop the stool from creating more tunnels. As the wound nears the surface, either a fistulotomy can be performed, or in time, the thread will fall out from the body. This method can take 3-6 months for the fistula to heal.
Medicated Seton Placement
Ksharasutra (Ayurvedic seton) is a thread coated with Ayurvedic medicine used to treat the fistula tract. The medicated thread (seton) is passed along the tract and tied snugly. The thread is changed every 2 weeks. While this non-surgical treatment is effective, with minimal post-operative pain and no risk of incontinence, it is currently not FDA-approved.
Platelet-Rich Plasma (PRP therapy)
PRP therapy is a newer treatment that injects platelet-rich plasma into the fistula to accelerate the healing process. PRP therapy is considered a last-therapy option for complicated or recurrent fistulas and must be combined with other treatments.
Fibrin Glue
This procedure injects special glue (made of blood-based products like fibrinogen and thrombin) into the fistula to seal the fistula closed. The results of this non-surgical procedure are poor.
At-Home Remedies to Heal a Fistula
First things first: A fistula will not and can not be healed solely by at-home or DIY remedies. Should spontaneous healing occur, the results of the ‘healed’ fistula will be temporary. The anal region is rife with bacteria, so without proper surgery, there is a high chance of reinfection and abscesses. However, the below remedies can help alleviate symptoms like itchiness, pain, and inflammation.
At-home fistula remedies include:
- Hydration: Drinking water and electrolyte beverages can loosen stools and prevent constipation. This encourages healthier bowel movements and relieves physical pressure on the fistula.
- Topical remedies: Coconut oil, oregano oil, olive oil, and aloe vera gel contain certain anti-properties (think antibacterial, antiviral, antibiotic, anti-inflammatory) that soothe the area following surgery.
Epsom salt: Soaking in an Epsom salt sitz bath can help soothe discomfort from fistulas, along with hemorrhoids, anal fissures, constipation or diarrhea.
Surgeries and Treatments for Fistulas
Fistula symptoms can be managed at home with non-surgical treatment, but surgery is necessary to close the abnormal passage. This is the only way for a fistula to heal. The most common surgery options include fistulotomy, fistulectomy, or seton surgery.
Other surgical methods include fibrin glue, a Surgisis plug, seton placement, laser fistula ablation, or an endorectal advancement flap. The latter procedures are reserved for complicated or recurrent fistulas.
Types of Fistula Surgeries
Fistulotomoy
Think about a pierced earlobe that can’t be stitched closed. Instead, a probe would likely be placed through the piercing. To open the area, a “V” shaped incision is made of the earlobe to the probe. As the ear heals over time the hole is closed. The same thing is done for a fistulotomy.
Once the anal fistula tunnel is identified, a “V” shaped cut is made, which removes the skin and tissue. This turns the tunnel into an open canal. Over the next 6-8 weeks, the scar tissue acts like natural cement and fills the open wound as part of the body’s natural healing process.
For more complex fistulas involving a lot of muscle, a cutting seton may be necessary. In this surgical procedure, a rubber band-like strip is wrapped around the muscle and tightened. The rubber band slowly cuts and loosens the muscle. After 2 weeks, the band is tightened again and cuts through the rest of the muscle before falling out with a bowel movement. This relatively slow procedure allows the muscle time to heal and stay intact, lowering the risk of incontinence.
The side effects of a fistulotomy include leaking of gas or stool. Since the fistula travels through the sphincter muscles, the risk of incontinence increases if too much muscle is cut. Success rates of fistulotomy are 98%, making it the most effective option for fistula surgeries.
Fistulectomy
Fistulotomy involves the surgical removal of the fistula tract in its entirety. This is not as effective as a fistulotomy.
LIFT or Ligation of the Intersphincteric Fistula Tract
This procedure involves making a small incision in the skin and using a probe within the fistula tract to locate the fistula within the intersphincteric plane. The doctor will then tie off and cut the tract within the intersphincteric groove, clean out the proximal tract, and close the tract and wound. This has less risks of the small risk of incontinence with a fistulotomy. As a proctologist, I do not perform LIFT procedures as the results are average at best, with a higher rate of recurrence than a fistulotomy.

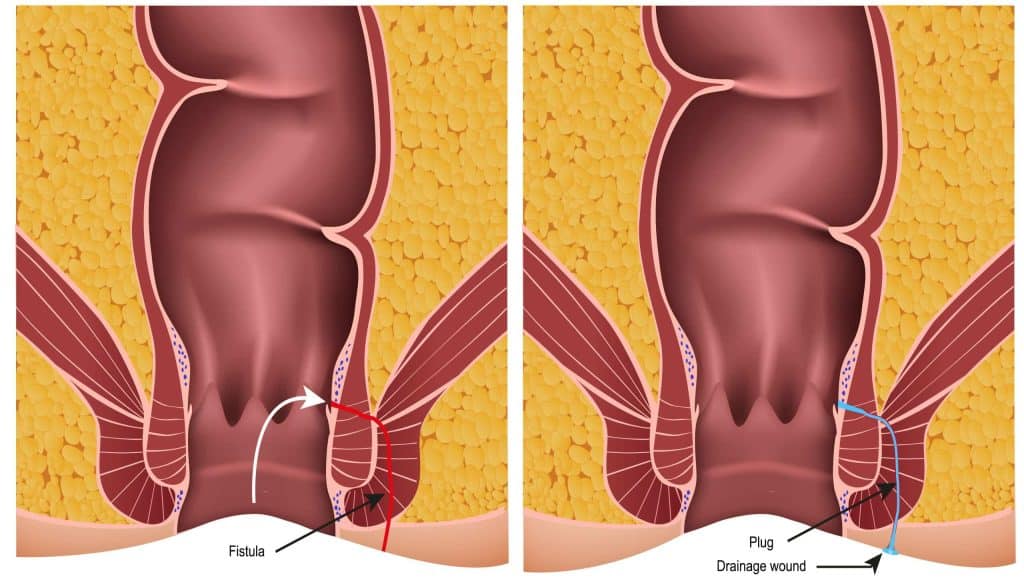
Fistula Plug
A fistula plug is a cone-shaped bioabsorbable material used to plug the fistula tract. The inner anal opening is closed with stitches over the plug. This surgical procedure can be repeated, if necessary, and poses no risk of incontinence. As failure rates are high (44%), I only recommend this procedure to patients with complex fistulas or fistulas related to Crohn’s disease.
Endofistula Laser Ablation of Anal Fistula
First, a laser fiber is placed along the fistula tract. As the fiber is removed, the laser heats the fibrous tract allowing it to heal. The inner opening is closed with stitches and failure rates are around 33%.
Endorectal Advancement Flap
During this procedure, a healthy piece of tissue is removed from the rectum and used as a ‘flap’ to cover the internal opening. This procedure is a backup option when regular surgery isn’t effective, such as treating Crohn’s related fistulas.
Benefits of Fistula Surgery
While surgery can be daunting, there are many benefits to choosing surgery over non-surgical, or therapeutic options.
- Fistulas rarely heal without surgery.
- The chance of the fistula returning after surgery is low—about 2%.
- Without surgery, recurrent infections and persistent drainage is common. The infections can become severe (Fournier’s gangrene), requiring emergency surgery.
- Without surgery, there is a small risk of developing cancer in the chronic untreated fistula tract.
Risks of Fistula Surgery
No surgery is completely risk-free. While fistula surgery carries a risk of infection and incontinence, the risk of complications is relatively low. Your personal level of risk depends on factors like age, allergies, the type of operation, and the location of the fistula.
The main risks of fistula surgery are:
- Severe Bleeding: Light bleeding or spotting is normal, but heavier blood loss can occur.
- Infection: All surgeries carry a risk of infection, and fistula surgery is no exception. To note: Thousand Oaks Proctology does not prescribe pre-procedure antibiotics.
- Incontinence: The likelihood of post-surgery incontinence is low, although this does depend on the type and location of the fistula.
- Recurrence of the fistula: If the fistula never properly healed, it will likely return. This is why I encourage patients to undergo surgery.
- Anesthesia complications: In rare cases, patients may have adverse reactions to anesthesia.
- Stroke: This is a more serious side-effect of Intracranial dural arteriovenous fistulas (DAVFs), which are fistulas that disrupt the blood flow.
In rare cases, fistula surgery can lead to blood clots, heart attack, pulmonary embolism, or even death. This depends on the complexity of the procedure or patients’ pre-existing health status.

FAQs About Fistulas
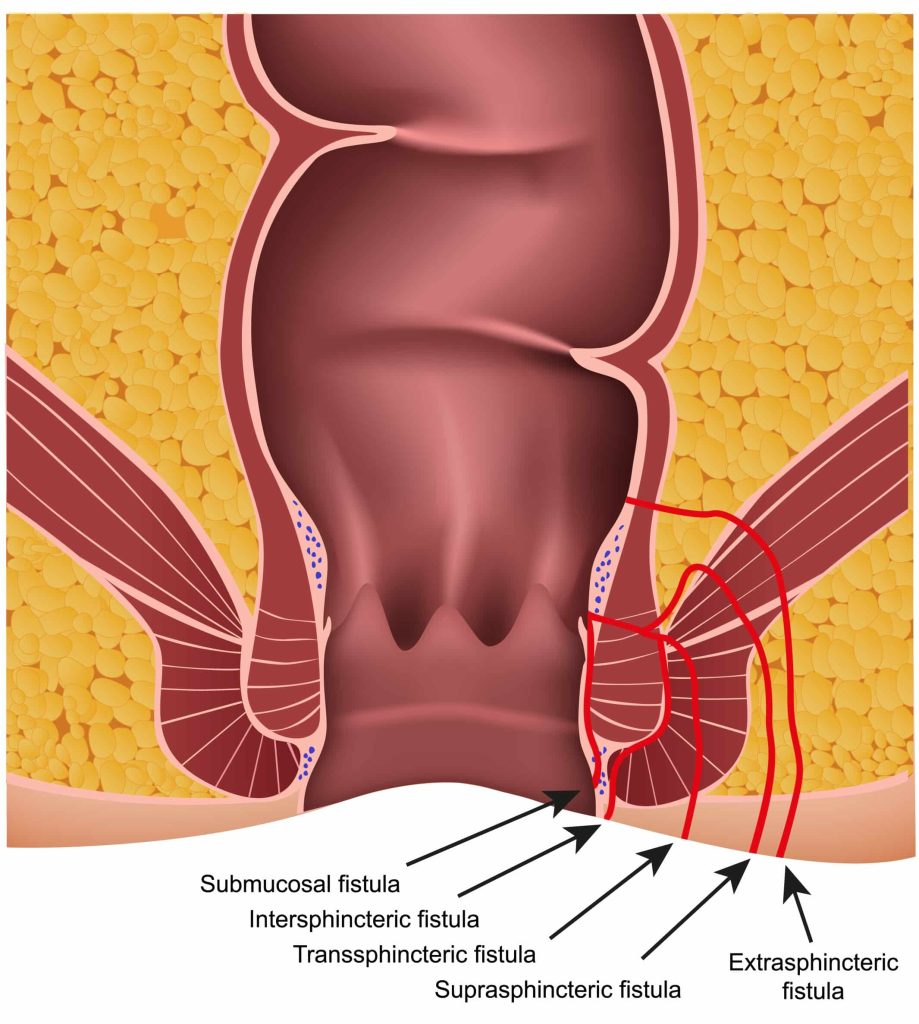
What are anal fistulas? Anal fistulas are abnormal tunnels that form between the inside of your anal canal to the skin outside.
What are the main symptoms of anal fistulas? The symptoms of anal fistulas will vary depending on the location and severity of the condition. However, common symptoms include rectum pain and swelling, discharge, recurring abscesses, uncomfortable bowel movements, and fever if the fistula is infected.
How do anal fistulas develop? Most anal fistulas are caused by an infection that clogs the anal gland. The glands secrete mucus to lubricate the anus to help the stool slide out, however, when the stool blocks the crypt, an abscess forms.
In some cases, the abscess will need to be surgically drained. Once drained, there is a 50/50 chance of a fistula forming between the inside crypt and the outside opening where the abscess drained.
Can Crohn’s disease cause fistulas? Yes, fistulas, which are caused by inflammation, are common in Crohn’s disease patients. Crohn’s is an inflammatory disease of the bowel and anus.
Can my doctor treat fistulas? If you experience any of the above symptoms, start by making a doctor’s appointment. Since there is no ‘one-size-fits-all’ approach to treating fistulas, anal or rectal problems, seeing a specialist is non-negotiable.
Most proctology issues fall outside the scope and expertise of general practitioners. That’s why your doctor will likely refer you to a proctologist or a colorectal surgeon. Proctologists are specialists trained in a variety of surgical and non-surgical procedures.
When to See a Doctor for a Fistula
If you notice unusual symptoms such as an anal lump, bleeding, discharge, pain, prolapse, or itching, it is important to book an appointment with a doctor for an evaluation.
It’s always tempting to dabble in DIY treatments, but in the case of anal fistulas, your condition will not heal without some expert medical intervention. Although there are risks to surgery, there are greater risks to avoiding surgery. For one, avoiding surgery increases the chances of cancer developing in the fistula.
If you’re concerned you have an anal fistula, contact our office today. We combine compassionate care with a pinch of humor. Contact us today to get to the bottom of your problems.

