A fistula is a communication similar to a small tunnel between the anus and the outside skin. A primary hole exists just inside the anus which is the beginning of a tract or tunnel that leads to a hole outside of the anus. It is similar to an ear piercing. There is a hole on the front of the earlobe and a hole on the back of the earlobe.
Many patients wonder how to heal a fistula without surgery, but the truth is that most will need surgery in order to be fully healed.
How Do Fistulas Develop?
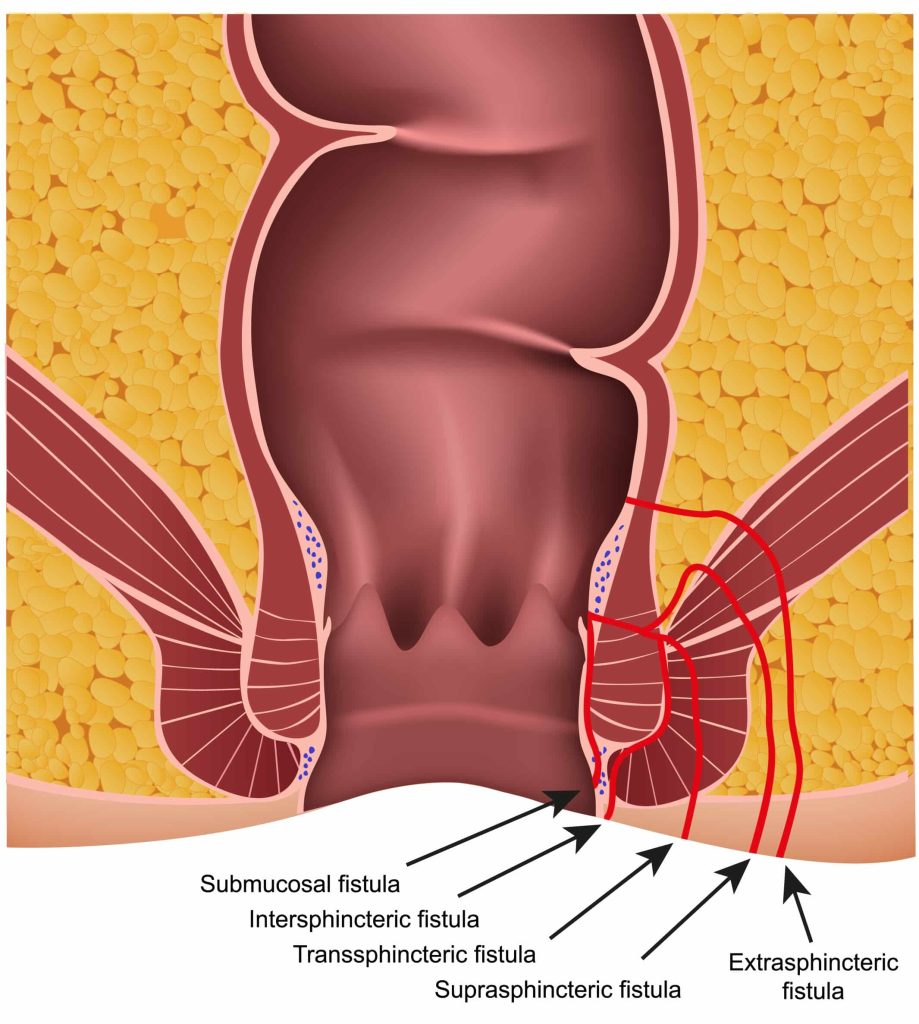
One type of fistula is called a cryptoglandular fistula. The inside of the anus is lined with 4 – 6 crypts (holes) which are connected to glands. The glands secrete mucus to lubricate the anus to help the stool slide out. When the crypt becomes blocked with stool, the gland becomes infected leading to an abscess.
The abscess can drain spontaneously. If it does not drain on its own, it will need to be surgically drained, usually at the skin level outside the anus. Once the abscess is drained there is a 50/50 chance of forming a fistula or a tract between the inside crypt and the outside opening where the abscess drained. Crohn’s disease, an inflammatory disease of the bowel and anus, is another cause of an abscess and fistula.
Symptoms of Anal Fistulas
Symptoms of anal fistulas will vary depending on the location and severity of the condition in a patient. Common symptoms of anal fistulas include:
- Pain and swelling in the same spot around the anus
- Swelling with discharge from the same spot at the anus
- Recurring abscesses in the same spot
- Pain or discomfort with bowel movements
- Fever, if the fistula is infected
Anal Fistula Treatments
It is very rare for a fistula to heal spontaneously or on its own. In order to heal, the internal opening must be obliterated and therefore surgery is necessary. Of the options to obliterate the internal opening, a fistulotomy or fistulectomy is one of the best.
Other methods include fibrin glue, a Surgisis plug, seton placement, laser fistula ablation, or an endorectal advancement flap. The latter procedures are reserved for complicated or recurrent fistulas.
Types of surgery
Fistulotomoy
Let’s go back to the earlobe explanation. If we wanted to close the hole created by the piercing and we couldn’t just close the hole with a stitch, a probe is placed through the piercing and a “V” shaped cut of the earlobe to the probe would open the area. As the ear heals over time the hole is closed. The same thing is done for fistula surgery.
In the operating room, the tunnel is found with a probe and then a “V” shaped cut is made which removes the skin and tissue below the skin which includes fat and muscle. This turns the tunnel into an open canal. The tunnel is then cleared out. The body will fill the open wound with scar tissue which acts like cement. The scar tissue grows from the deep portion of the canal to fill the open tunnel. This process takes 6-8 weeks.
The majority of fistulas are simple and require either opening the tract or removing the tract and obliterating the internal opening (fistulectomy). One small risk of a fistulotomy includes leaking of gas or stool after the surgery. Since the fistula travels through the sphincter muscles, if too much muscle is cut, the risk of incontinence increases. This risk is about 3-5%.
Prior to opening the fistula tract, the amount of muscle within the tract is observed and if a majority of the sphincter muscle is traversed by the fistula, a seton, or rubber band, will be placed instead of surgically dividing the muscle. The seton cuts through the sphincter muscle over a period of weeks allowing the muscle to be divided without losing its integrity. The seton is tightened in the office every 2-3 weeks until it falls out. Placing a seton decreases the risk of incontinence.
Success rates of fistulotomy are 98%, making it the most effective option of fistula surgeries.
Lift or ligation of the fistula
Ligation of the Intersphincteric fistula tract; this treatment involves making a small incision in the skin and using a tool to locate the fistula. Once the fistula is located, the doctor will tie off the tract and remove the infected tissue to help recurrence. For me, the results are average at best with a higher rate of recurrence than a fistulotomy, and so I personally do not perform the LIFT procedure.
Fibrin glue
Special glue made up of blood-based products like fibrinogen and thrombin. The glue is injected into the fistula which was supposed to seal off the fistula and inner opening to heal the fistula. The results were very poor and are no longer used to treat anal fistulas.
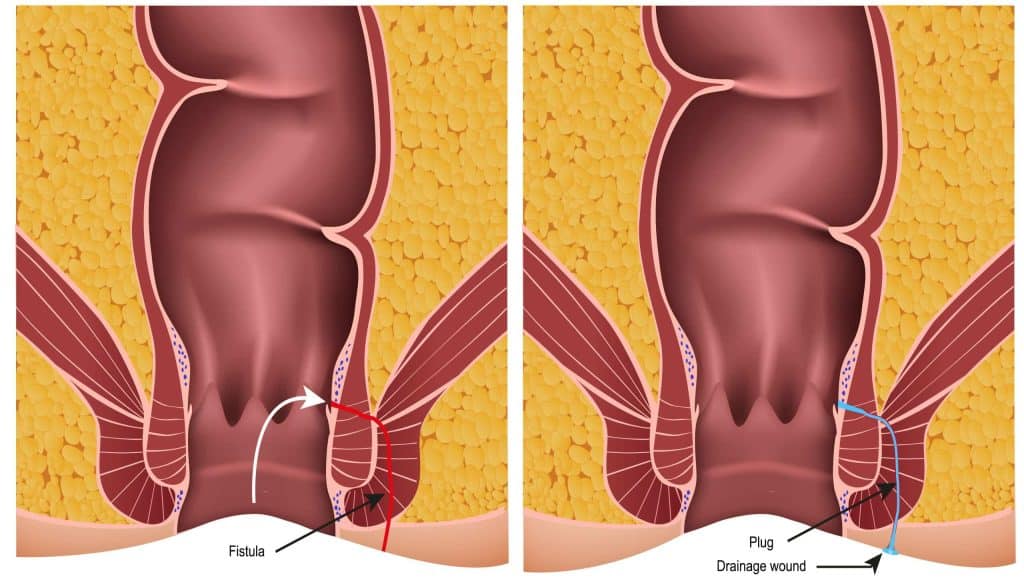
Fistula plug
A fistula plug is a cone-shaped bioabsorbable material used to plug the fistula tract. In surgery, the surgeon finds the fistula tract and pulls the cone-shaped plug into the tract. The inner anal opening is closed with sutures over the plug. Advantages are that there is no risk of incontinence and can be repeated if it fails. For me, it is a good procedure for patients with complex fistula or patients with Crohn’s disease and fistulas related to Crohn’s disease. Failure rates are 44% or higher. In my experience and the experience of my colleagues, it has been very poor so I have abandoned using the fistula plug.
Endofistula laser ablation of anal fistula
A laser fiber is placed along the fistula tract and as the fiber is removed from the tract the laser is used to heat the fibrous tract allowing it to heal. The inner opening is closed with sutures. Failure rates are up to 33%.
Endorectal advancement flap
During this procedure, a healthy piece of rectal mucus elevated and brought down to cover the internal opening. This is used for patients with Crohn’s related fistulas as a regular fistula surgery will not work and can make the problem worse.
How to heal a fistula without surgery
Non-medicated seton placements (cutting and non-cutting setons)
For Crohn’s disease, a small piece of surgical thread is placed through the fistula to help the fistula stay open and control the tract. This is a non-cutting seton. Crohn’s related anal fistulas come from severe inflammation and the goal is to keep stool from creating more tunnels. Placing a thread (drain) along the tract allows for control of the fistula to prevent recurrence.
For complex cryptoglandular fistulas, a small piece of surgical thread is placed through the fistula to help the fistula heal. This is a non-cutting seton. The patient is instructed to spin the thread within the fistula to promote inflammation. Since the thread is a foreign body, the process of healing pushes the wound to the surface. As the wound gets closer to the surface, either a fistulotomy can be performed, or in time the body will push the thread out of the body, and the fistula will heal. The process can take 3-6 months to heal.
For complex deep fistulas, a cutting seton can be placed. A rubber band-like strip is wrapped around the muscle and tightened at the time of surgery. The rubber band slowly cuts the muscle, and in 2 weeks, it is loose. In the office, it is tightened again, and it slowly cuts through the rest of the muscle and falls out with a bowel movement. As the band is cutting the muscle very slowly, the muscle can heal behind the band, so the muscle stays intact, and there is less risk of incontinence.
Medicated seton placement
Ksharasutra (Ayurvedic seton) is a medically treated thread using Ayurvedic medicine, including herbal medicines, used to treat the fistula tract. The tract is identified at surgery, and the medicated thread (seton) is passed along the tract and tied snugly. The thread is changed every 2 weeks and tied snugly after it is changed. Advantages of this therapy are that the procedure works very well, there is minimal post-operative pain, and there is no risk of incontinence. The main issue is that the medicated thread is not FDA approved, so it cannot be used in the United States.
Platelet-rich plasma (PRP therapy)
A newer treatment; this treatment injects platelet-rich plasma into the fistula to promote healing. The inner opening is closed with a mucosal advancement flap. This process is used for complicated or recurrent fistulas. Recurrences are up to 16%.
Benefits of Fistula Surgery
Although you might be wondering how to heal a fistula without surgery, the most effective treatment for fistulas is surgery by a professional. While surgery may seem daunting, there are many benefits to choosing surgery over other options.
- Fistulas rarely heal without surgery.
- The recurrence rate (chance of the fistula coming back) after surgery is about 2% (very low).
- Without surgery recurrent infections and persistent drainage is common. The infections can become severe (Fournier’s gangrene) requiring emergency surgery.
- Without surgery, there is a small risk of developing a cancer in the chronic untreated fistula tract.
Risks of Surgery
- Severe Bleeding 1-2%
- Infection 1-2% (I do not prescribe pre-procedure antibiotics)
- Incontinence (very low)
- Recurrence of the fistula
- Depending on the surgery it can be as low as 2% or higher than 44%. Fistulotomy has the lowest recurrence at 2%.
- Anesthesia complications (rare)
- Stroke
- Clots in the legs
- Heart attack
- Pulmonary embolism
- Death
When to See a Doctor

It is important to remember that fistulas will not heal without some sort of procedure. Although there are risks to surgery, there are also risks with avoiding surgery. One very small risk of not doing surgery is the chance that cancer develops in the fistula. Therefore, if you are diagnosed with a fistula-in-ano, surgery is the treatment of choice. For symptoms such as an anal lump, bleeding, discharge, pain, prolapse, or itching, it is important to see your doctor for an evaluation.

