Pilonidal dimples, also known as pits, are subtle indentations or small holes located just above the buttocks at the base of the spine. Despite their shallow nature, these dimples often go unnoticed and are sometimes mistaken for sacral dimples, which are generally harmless skin indentations without associated issues. It’s crucial to distinguish between the two, as sacral dimples are usually innocuous, while pilonidal dimples can lead to medical concerns.
Sacral dimples, if large and noticeable from birth, may warrant attention, as they could signal an underlying spinal issue, necessitating evaluation by a healthcare professional. Conversely, pilonidal dimples refer to a condition where a small pit or hole in the skin near the tailbone becomes infected or accumulates debris, such as hair. It’s important to note that although a small percentage of individuals born with pilonidal pits may also have spinal abnormalities, the majority do not experience such complications. Recognizing the distinction between these conditions allows for appropriate medical assessment and intervention when needed.
Recognizing a Pilonidal Dimple
Pilonidal dimples, sometimes called pilonidal pits, are typically found in the midline, between the buttocks, near the tailbone. They are often a pit or depression on the skin and can be shallow or deep. They may even look like a small hole at the top of the buttocks.
There may be hair in and around the dimple. In some cases, hair may be trapped beneath the skin which can lead to a pilonidal cyst forming.
Pilonidal Dimples vs. Sacral Dimples
It is easy to mix up the two, but a pilonidal pit and a sacral dimple are different conditions in the same area. Sacral dimples are small indentations or pits located at the base or the spine, but they are present from birth and are generally harmless.
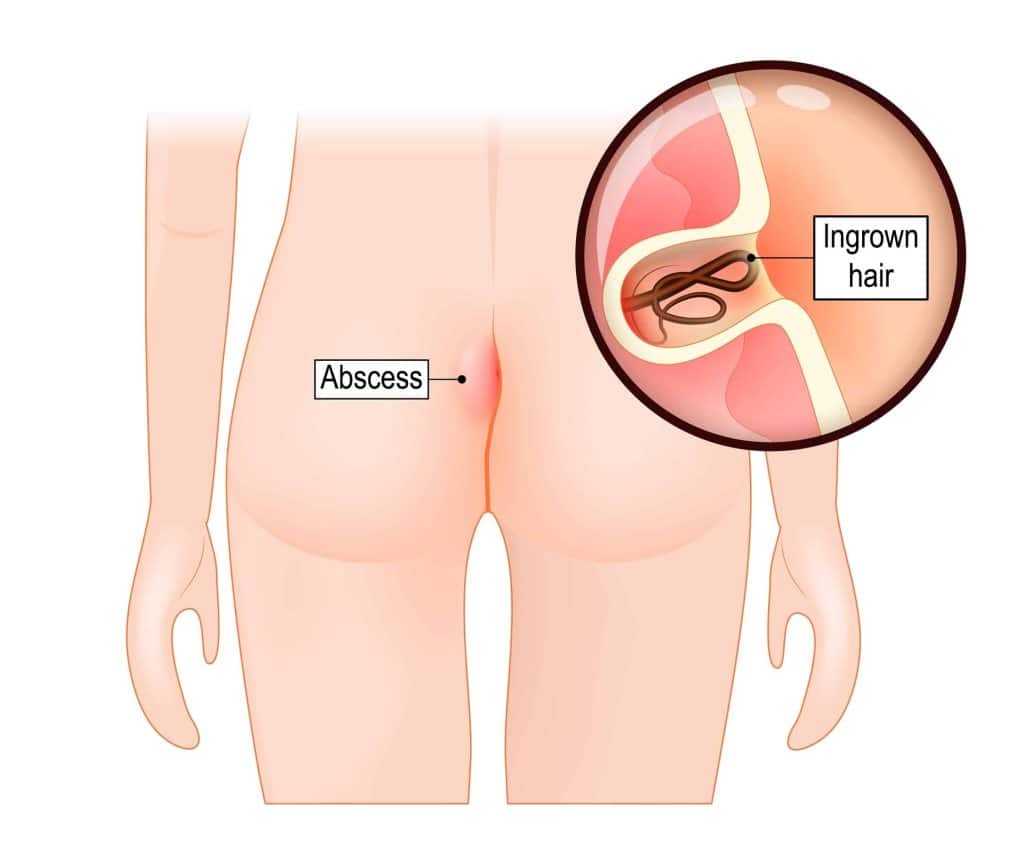
Pilonidal dimples are also small and found in the sacral region, but they are associated with pilonidal cyst disease which I feel comes from tailbone trauma and is not congenital. Pilonidal cyst disease is when a small pit of dimple becomes infected which leads to the formation of a cyst or access.
Pilonidal cysts can form when the dimple has fluid and hair trapped and accumulates. When the cyst becomes infected, leading to an abscess at a distance from the original offending pit, it is either drained in the office or ruptures on its own. Once it ruptures or is drained by a proctologist, it will lead to a sinus tract.
If you have a sacral dimple without any symptoms, it is likely benign. However, if you experience pain, swelling, or other concerning symptoms in the sacral region, it’s essential to seek medical attention for proper evaluation and diagnosis.
Are There Treatment Options for Pilonidal Dimples?

Pilonidal dimples on their own usually do not need treatment. However, if there is pain in the region, pus drainage, or redness, it is important to seek out medical care from a proctologist as a pilonidal sinus or cyst may have formed.
Treatment options for pilonidal cysts depend on the severity of the condition:
Observation
When a pilonidal dimple is asymptomatic, proctologists often recommend a cautious, observational approach without immediate action; it’s often better to wait and see what happens rather than undergo an unnecessary procedure. This is best when the pilonidal dimple isn’t causing any symptoms and there isn’t an urgent need for medical attention. Regular monitoring allows healthcare professionals to assess any changes in the condition over time and decide on further actions if necessary.
Antibiotics
If a pilonidal dimple is infected, your proctologist will prescribe antibiotics to get rid of the infection. Antibiotics can reduce inflammation, combat bacteria, and promote a favorable environment for the body’s natural healing processes.
Incision and drainage
When an abscess forms within the pilonidal cyst, your proctologist may opt for an incision and drainage procedure. This surgical intervention involves making an incision to release accumulated fluids and facilitate the drainage of pus. Incision and drainage are vital for relieving pressure, addressing infection, and accelerating the healing process, particularly in cases where there is a localized collection of fluid. Incision and drainage for pilonidal cysts are typically done such as a doctor’s office and may be in an outpatient setting.
Hair removal
Maintaining good hygiene and cleanliness in the affected area is essential for preventing complications associated with pilonidal cysts. Some healthcare providers may recommend the removal of hair in the affected region through waxing or laser-hair removal. This preventive measure aims to decrease the risk of hair becoming trapped, a factor that can contribute to the formation and recurrence of pilonidal cysts. Regular hair removal practices may be advised to reduce the likelihood of future episodes.
Surgical excision
For recurrent or severe cases of pilonidal cysts, surgical excision becomes a consideration. This more invasive approach involves the complete removal of the pilonidal pit, sinus, or cyst. Surgical excision aims to eliminate the source of the problem, reducing the likelihood of future recurrences and complications. This option is often explored when conservative measures prove insufficient or when there is a persistent and significant impact on the patient’s quality of life.
A healthcare provider can assess the condition, determine the appropriate course of action, and discuss treatment options tailored to the specific situation. Self-diagnosis and self-treatment are not recommended, as pilonidal disease can vary in severity, and professional guidance is crucial for effective management.
Tips for Managing Pilonidal Disease
Although having a pilonidal pit may not lead to pilonidal disease, there are some ways to cut your risk factor. These include a combination of self-care and medical care.
Maintain good hygiene
Regular cleansing of the affected area is paramount. Thorough and gentle cleaning helps prevent the accumulation of debris, bacteria, and hair, reducing the risk of infection and inflammation.
Hair removal in the area
Keeping the area around the pilonidal pit hair-free is crucial. Hair removal diminishes the chance of hair becoming trapped in the dimple, a common trigger for pilonidal cyst formation.
Avoid sitting for too long
Prolonged periods of sitting can contribute to irritation and pressure on the pilonidal area. Taking breaks, standing, and moving around can alleviate stress on the affected region.
Use cushions
Opting for flat foam pads rather than donut-shaped cushions is recommended. Donut cushions may exert excessive pressure on the pilonidal area, potentially exacerbating discomfort and contributing to complications.
Regular inspections
Periodically inspecting the pilonidal area for any signs of redness, swelling, or discharge is essential. Early detection of changes allows for timely intervention and prevents the progression of the condition.
Avoid tight-fitting clothing
Loose-fitting clothing helps reduce friction and irritation around the pilonidal pit. Tight clothing can aggravate the area, potentially leading to increased discomfort and a higher risk of complications.
Maintaining a healthy diet and getting enough fiber
A balanced and fiber-rich diet supports overall health and can contribute to regular bowel movements. Avoiding constipation is crucial, as straining during bowel movements can strain the pilonidal area.
Keep a healthy weight
Maintaining a healthy weight is beneficial for overall well-being and can contribute to reducing the risk of complications associated with pilonidal disease.
Remember that the management of pilonidal disease varies from person to person, and individualized treatment plans are crucial. It’s essential to work closely with a healthcare professional, like Dr. Rosenfeld of Thousand Oaks Proctology, who can assess your specific situation and provide appropriate guidance and treatment.

