Hemorrhoid vs Polyp
Colon health is too often swept under the rug. As part of the digestive system, the colon’s main job is eliminating what the body does not digest. The colon converts liquid stool into solid stool by absorbing water and dehydrating it as it passes. Besides absorbing water, the colon also plays a role in electrolyte balance.
A healthy colon means a healthier you. When it’s working correctly, there is less risk of colorectal and anorectal issues such as diverticulosis, hemorrhoids, anal fissures, anal fistulas, perirectal abscesses, and anal itching, to name a few. But many things can go wrong with the colon.
Eating a healthy diet rich in fiber along with fiber supplements, like PERFECT P.O.O.P. raw psyllium fiber (prebiotics), plus fermented foods (probiotics) boosts our immunity and reduces toxic inflammation. This diet can lower the risk of conditions like dementia, Alzheimer’s disease, and metabolic syndrome (high blood pressure, blood sugar, cholesterol, lipids, and obesity).
Most of us will deal with common colon issues like constipation or diarrhea, including Irritable Bowel Syndrome (IBS). While these might not be causes for serious alarm, there are other more severe colon conditions.
Differences Between Hemorrhoids and Polyps
The question “Is a hemorrhoid a polyp?” confuses many people. In short, the answer is no. Hemorrhoids and polyps are two distinct medical conditions with different treatment options.
What are Hemorrhoids?
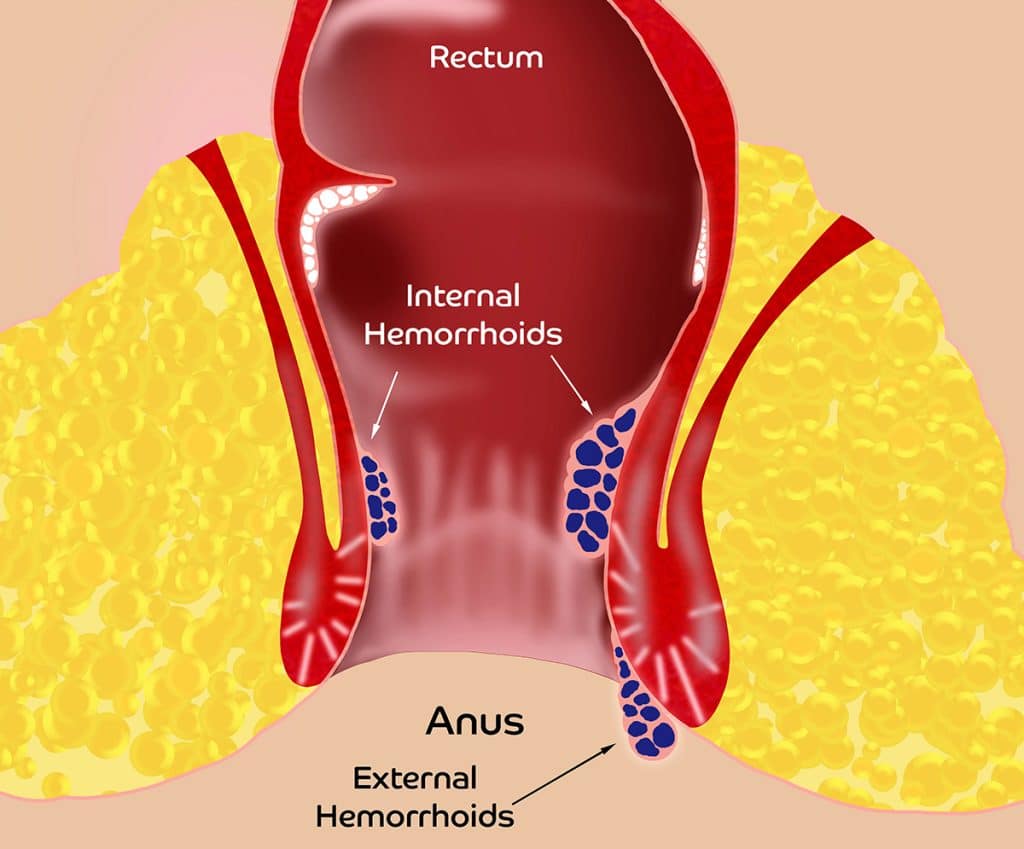
Hemorrhoids are blood vessel cushions located inside and outside the anus. Every person is born with approximately six hemorrhoids – three internal and three external. These vascular cushions have both arterial blood supply and venous drainage, and may help prevent stool leakage, though their exact purpose remains unproven.
Hemorrhoid problems occur when these vessels become inflamed and enlarged. During inflammation, proteins in the blood cause it to thicken, making it harder for blood to flow out of the hemorrhoid while blood continues flowing in. This condition, called chronic venous insufficiency (CVI), causes the hemorrhoid to swell – similar to a water balloon that fills faster than it can drain. As hemorrhoids enlarge, they can become symptomatic, a common condition affecting millions of people.
Symptoms of Hemorrhoids
Hemorrhoids can be internal or external, each with distinct symptoms. While hemorrhoids can cause pain, it typically manifests as a throbbing or aching sensation, unlike the sharp pain associated with anal fissures.
Internal Hemorrhoid Symptoms:
- Aching pain around the anus
- Painless bleeding
- Anal itching and pressure
- Tissue prolapse (protrusion outside the anus)
- Mucous discharge
- False urgency to have bowel movements
- In severe cases, tissue death (necrosis), which requires emergency surgery
External hemorrhoid symptoms:
- Blood clots (thrombosis), which appear as painful purple lumps. Thrombosed hemorrhoids resolve on their own 95% of the time. Recurrence in the same spot is unlikely, so conservative therapy is typically recommended.
- Swelling without clotting
- Necrosis can also happen with external hemorrhoids, also requiring emergency surgery
Hemorrhoids can often be managed with lifestyle changes, dietary adjustments, and over-the-counter treatments such as topical creams, ointments, or suppositories.
Hemorrhoid symptoms can be misleading. People may either overreact to minor cases or, more dangerously, dismiss serious colon health issues as simply being hemorrhoids. Since this confusion can have life-threatening consequences, it’s crucial to get proper medical evaluation rather than self-diagnosing. At Thousand Oaks Proctology, we encourage people to educate themselves so they don’t make this mistake. This knowledge may one day save your life.
As with any health condition, the experts always know best. Doctors, especially proctologists, are trained to distinguish between hemorrhoids and polyps.
What are Polyps?
Polyps are abnormal growths on the lining of the colon or rectum that can develop into cancer, unlike hemorrhoids, which are non-cancerous vascular structures. While polyps rarely bleed unless they’re large, any rectal bleeding should be evaluated seriously since colon cancer rates are increasing dramatically in people under 45. Unfortunately, both patients and doctors sometimes dismiss bleeding as “just hemorrhoids” without proper investigation, leading to delayed diagnosis of more serious conditions.

Large polyps, particularly those near the rectum, can mimic hemorrhoid symptoms by protruding during bowel movements and causing bleeding or mucous discharge. However, most polyps develop without any warning signs, so it’s crucial to get a colonoscopy when rectal bleeding occurs, even if it seems minor or temporary. This fundamental difference from hemorrhoids – the potential for malignancy – makes proper medical evaluation essential.
Most people with colon polyps don’t even know they have them. So, how can they then be vigilant in reducing their risk?
How to Prevent Hemorrhoids and Polyps
Hemorrhoid prevention includes a healthy diet of up to 30 grams of fiber daily. To meet this daily goal, I recommend my brand of fiber, PERFECT P.O.O.P. raw psyllium fiber. This supplement helps increase stool bulk, reducing the need to strain during bowel movements and minimizing the time spent sitting on the toilet.
Polyp prevention includes a regular colonoscopy screening schedule. Routine colonoscopies decrease the risk of colon and rectal cancer death by 53%. The industry recommends that the average person start screenings at age 45.
How and why polyps form is still a mystery, but it’s believed that environmental factors, like toxins in the air and food, may play a role. Genetic susceptibility to colon polyps is also possible, though only 5% of colorectal cancers are linked to genetics. Age and lifestyle choices, such as diet and smoking, also contribute. While no one is entirely immune, avoiding a high-fat diet, low fiber intake, and smoking can help reduce the risk.
Treatment Options for Hemorrhoids and Polyps
If you’re dealing with hemorrhoids, the good news is you can often manage them on your own. If hemorrhoid symptoms begin, the recommended first step is to see a proctologist.
To help reduce hemorrhoid symptoms naturally, here are some things you can start right away.
- Add the supplement PERFECT P.O.O.P. raw psyllium fiber to your diet. This supplement bulks the stool making it easier to pass while lowering anal pressure and reducing hemorrhoid size.
- Start R.H.O.I.D. – AID. This supplement contains micronized Diosmin, a natural antioxidant and bioflavonoid that helps shrink hemorrhoids and alleviate symptoms.
- Start sitz baths with Epsom salts. Purchase a sitz tub from the pharmacy, fill it with warm to hot water and Epsom salts, and soak for 10-15 minutes, 3-4 times daily.
- Use over-the-counter hemorrhoid ointments
- Preparation H – Helps to lubricate and sooth the area.
- Vaseline – Helps to lubricate and sooth the area.
- Balenol – Helps to lubricate and sooth the area.
- Recticare, which contains 5% Lidocaine to lubricate and soothe the area. Apply every 2-3 hours for up to 4 days, but stop after 4 days to avoid skin irritation from prolonged use.

A proctologist can often treat external and internal hemorrhoids in their office. One of the most common treatments for internal hemorrhoids is sclerotherapy. This treatment involves an injection of 5% phenol mixed with olive oil into the internal hemorrhoid. Although it sounds painful, internal hemorrhoids lack the nerve endings sensing pain and temperature so it is painless! I know this for a fact as I had my hemorrhoids treated on 2 occasions. For external hemorrhoids that remain symptomatic, excision is necessary, which can also be done in the office with a recovery time of 3-7 days.
If you have bleeding, it is imperative to have a colonoscopy to rule out polyps and cancer.
The doctor will visually inspect your colon and rectum for abnormal growth during this procedure. If any cancerous rectal polyps are found, they will be removed immediately.
Colonoscopies seem scarier in theory. Since you’re sedated, the procedure is painless, though many people still dread them. While a colonoscopy might feel awkward, discomfort is a small price for a potentially life-saving procedure.
The Connection Between Polyps and Colon Cancer
The connection between hemorrhoids and polyps is not a direct connection. Hemorrhoids themselves do not lead to polyps or cause colorectal cancer. Hemorrhoid symptoms of bleeding require a colonoscopy. During a colonoscopy, polyps may be discovered and removed, which helps reduce the risk of colorectal cancer. This is an indirect connection between hemorrhoids and colon polyps.
About 1 in 3 people with a family history of colon polyps or cancer face an increased risk of colorectal cancer; however, people can minimize colon issues to an extent with regular screening colonoscopies and healthy lifestyle choices. Understanding the various risk factors, including age, diet, and lifestyle, can help individuals take proactive steps to reduce their risk.
The good news is that most polyps in the colon and rectum are harmless. Only about 5% of adenomas, the precancerous type of colon polyps, ever turn into cancer. Even though it can take 7-10 years for adenoma to develop into cancer, it’s not worth risking it. Your individual risk level is impossible to predict.
Colon polyps morph into cancer via continued mutations in the cell DNA. These mutations create out-of-control cells that grow and divide to form a tumor. Unchecked polyps keep growing and can eventually turn into cancerous tumors that spread to other parts of your body. That’s why identifying and removing polyps early is imperative.

While hemorrhoids are the usual culprits behind bleeding or rectal pain, and more common than cancer, it’s worth booking an appointment with a proctologist who will provide clarity and reassurance. Early detection is your best chance of cure. Plus, peace of mind is priceless.
When to See a Proctologist
Proctologists are experts in colon and rectal health. Most lower digestive tract issues are right “up their alley”. Proctologists, like Dr. Rosenfeld at Thousand Oaks Proctology, offer specialized services, such as colonoscopies, hemorrhoid treatments, and excisional hemorrhoid surgery, to address various colorectal health issues.
Most people with polyps won’t even know they have them since there are usually no symptoms. This invisible nature of polyps makes regular screenings and check-ups a priority for everyone.
So, when’s the right time to see a proctologist? If you notice rectal bleeding, a lump in the anal area, mucous discharge, anal itching, anal pain or any unusual changes in your bowel habits, it’s time for a proctology examination.
At Thousand Oaks Proctology, we are on top of our game to get to the bottom of your problems. Peace of mind is everything. Book your consultation today.

